Friday, 28 October 2022
Multi-volume overlapping ablation zone of a large metastatic liver lesion in segment VIII
Multi-volume overlapping ablation zone of a large metastatic liver lesion in segment VIII
3:23
Semmelweis University hospital performed their first CAS-One IR navigated ablation case on this patient with a large 41x37mm lung metastasis in the liver. Full ablation zone coverage of all margins was simulated and achieved by planning and placing three trajectories, to form four overlapping ablation zones. The needles were accurately placed and the post-ablation analysis confirmed A0 ablation of this large tumour. CAS-One IR streamlined and standardised the CT-guided ablation workflow for this otherwise complex case.
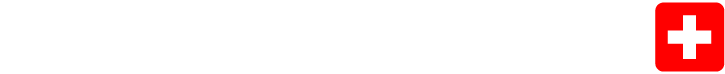
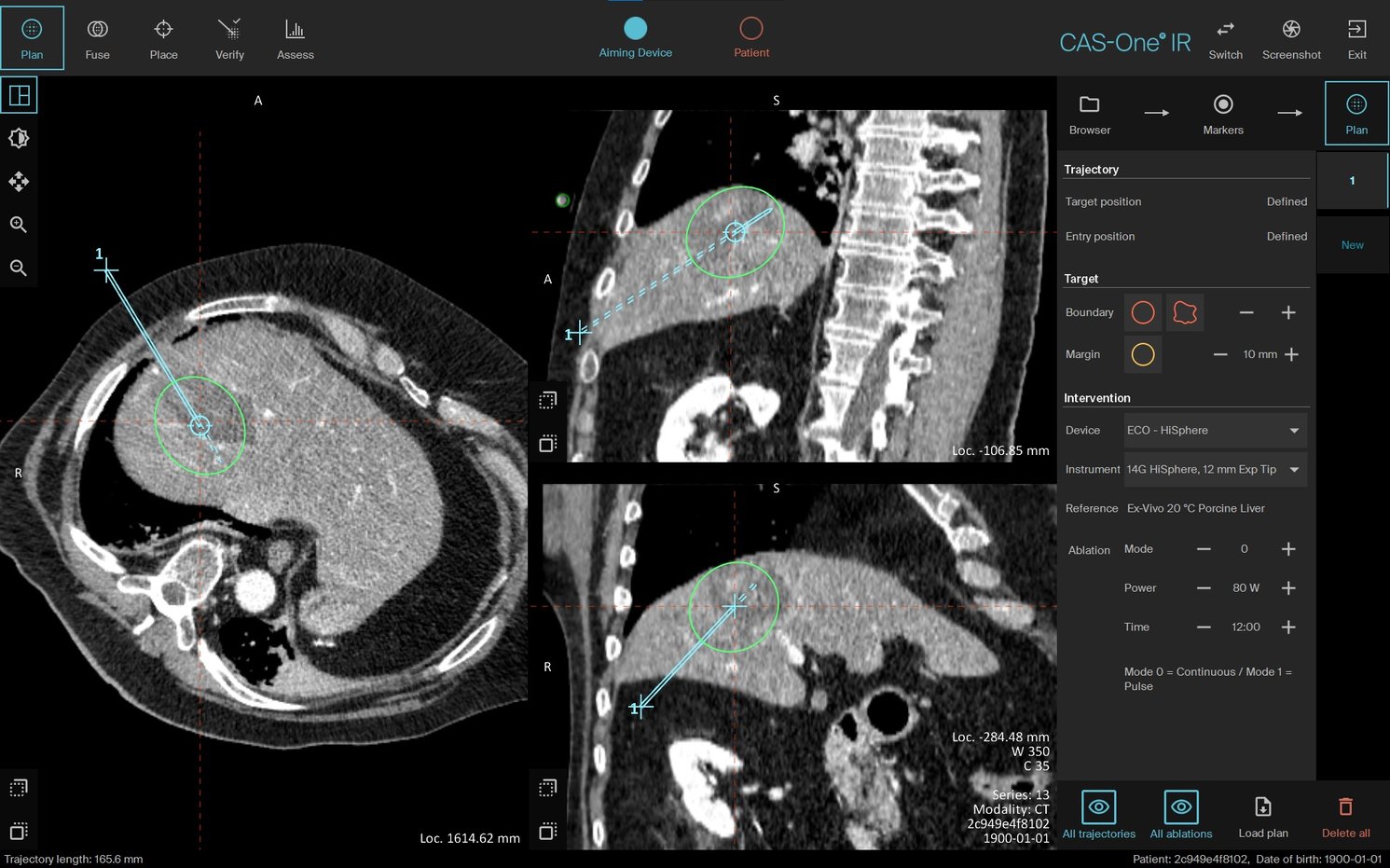
Plan with segmented tumour in red, safety margin in yellow, and the four overlapping ablation zones in green.
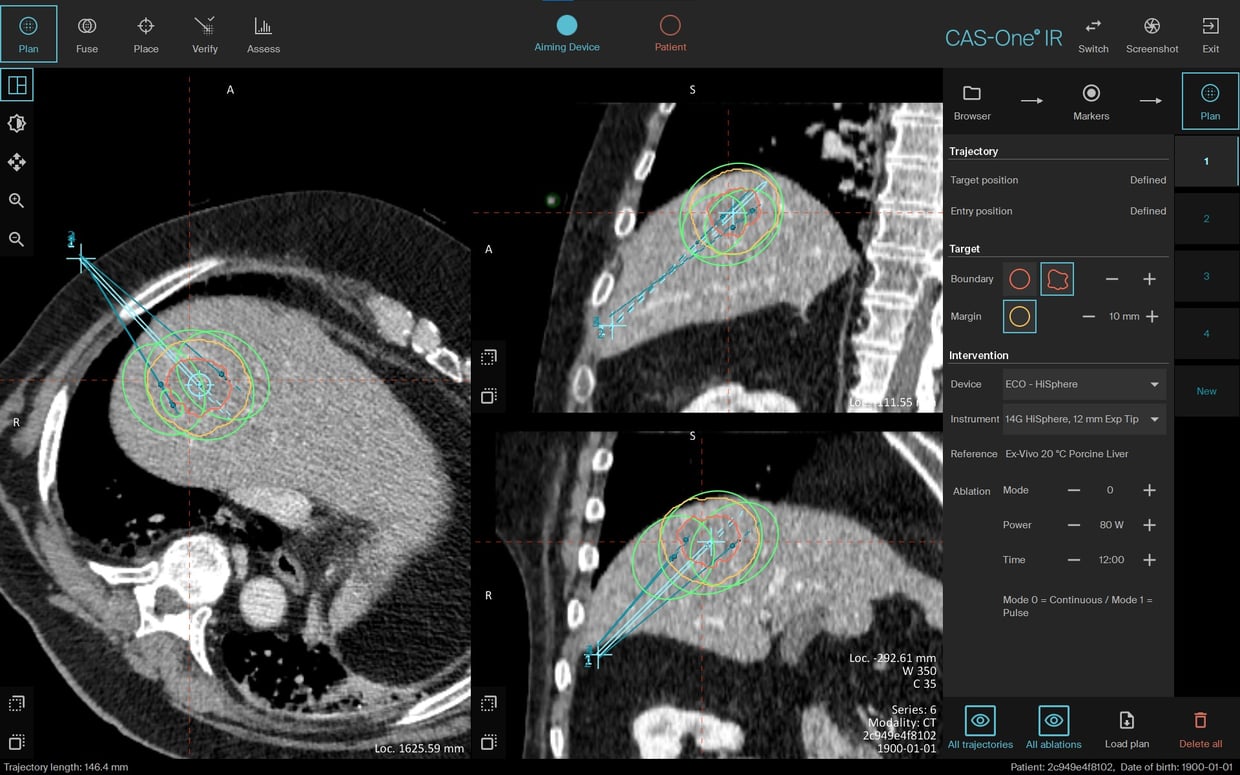
3D image reconstruction showing the trajectory view with the segmented tumour in red, 10mm safety margin in yellow and the overlapping ablation zones in green.
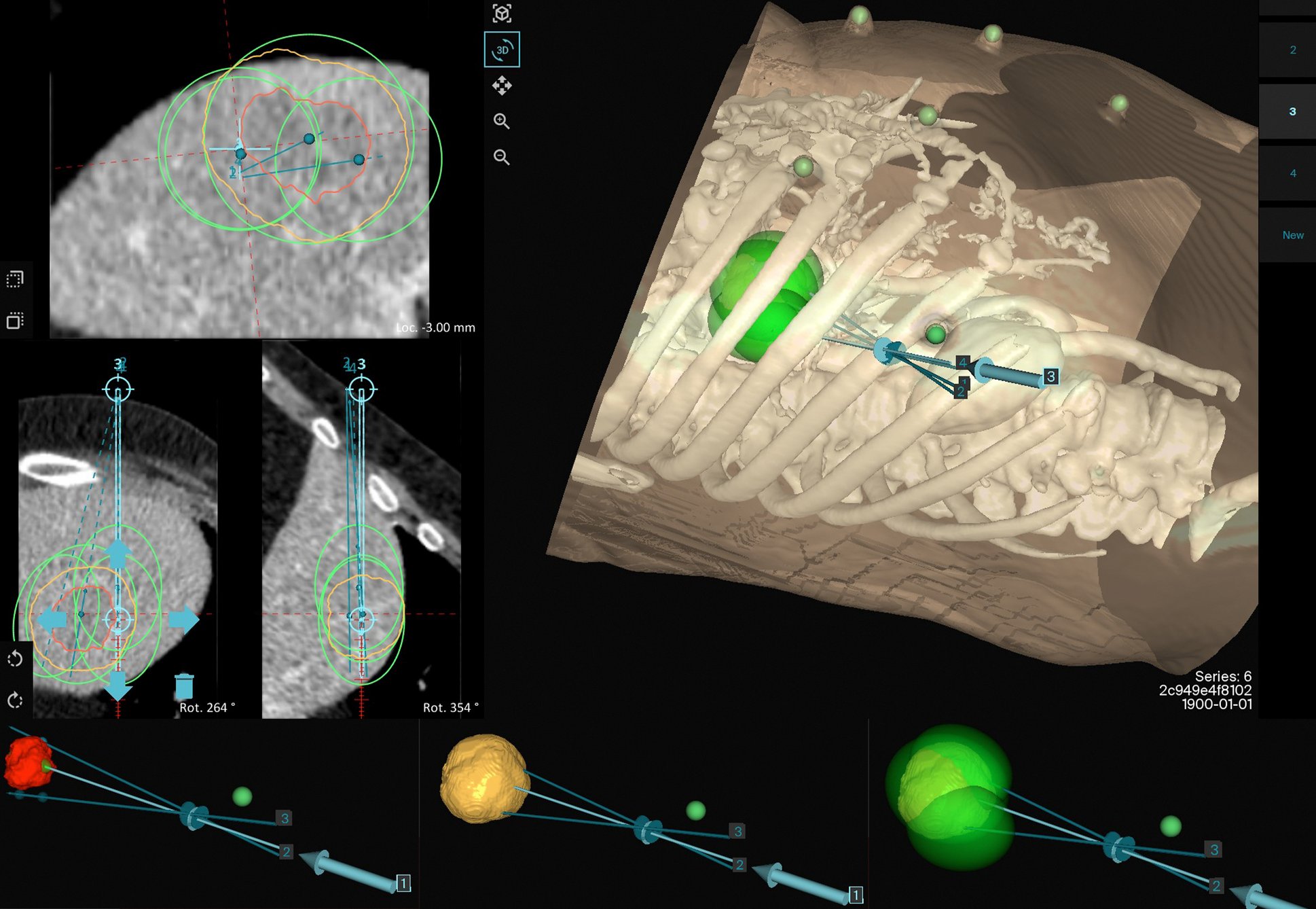
Post-ablation image with segmented ablation zone in green.
Re-ablation plan to boost coverage of the caudo-lateral section of the original ablation zone.
Name: Dr. Pál Ákos Deák MD. PhD.
Institution: Semmelweis University, Dept. of Interventional Oncoradiology, Budapest (Hungary)
Patient age and sex: 75 years, male
Initial condition:
- Patient was initially diagnosed with metastatic lung adenocarcinoma.
- Previous cerebellar metastasis was treated with stereotactic body radiation therapy (Cyberknife).
- Patient underwent multiple cycles of radio/chemo/immunotherapy.
- A 27x30mm Liver lesion was detected in July 2022 on an MRI scan and was subsequently biopsied. Histological analysis confirmed almost 100% HER2 positivity correlating with lung adenocarcinoma metastasis.
- The patient was referred for CAS-One IR navigated ablation for the treatment of this solitary metastatic liver lesion.
Treatment:
- Tumour size on the day of treatment had grown to 41x37mm.
- Due to the size of the tumour, an overlapping ablation zone treatment was planned with three trajectories forming four ablation zones (a pull back ablation was planned with one of the trajectories).
- Each needle was navigated to and post-placement analysis confirmed accurate needle advancement.
- The post ablation scan showed complete ablation of the tumour with a slight under-ablation of the safety margin.
- A new trajectory was re-planned and the patient was re-ablated to achieve full coverage of the safety margin following the first ablation.
- A subcapsular haematoma (about 5mm in width) was also formed, which was self limiting - confirmed by a later CT scan and followed later with Ultrasound.
Conclusion:
- This was the first CAS-One navigated ablation case performed by the centre.
- This complex ablation case was successfully treated with stereotactic navigated ablation using CAS-One IR.
- The planning and simulation of overlapping ablation zones through placing multiple trajectories was simplified and standardised using the CAS-One IR workflow.
- This technique would otherwise have been challenging using the conventional freehand technique, with a high risk of accuracy and efficiency being compromised.
- The operating physician was satisfied with the workflow and treatment outcome, and looks forward to continuing with CAS-One IR navigated cases.