Quantification of ablation margins is gaining importance in interventional oncology
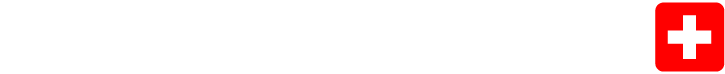
Quantification of ablation margins is gaining importance in interventional oncology. Typically, margins are quantified using annotations derived from co-registered pre- and post-ablation images, as described by Sandu and Paolucci et al. Annotations include both the tumor and the effectively treated volume (i.e. necrotic tissue), as well as the organ capsule for subcapsular lesions.
We want to highlight four interesting publications focusing on ablation margin quantification:
• A study from the team led by Dr. Bruno Odisio (MD Anderson, Houston, USA) has analyzed the impact of different registration techniques in the computation of ablation margins for predicting local tumor outcomes. The study supports the role of biomechanical deformable image registration to account for intraprocedural deformations of the target anatomy.
• Another report from the team at Mayo Clinic (Phoenix, USA) compared ablation zone volumes immediately at the completion (T = 0) of 26 microwave ablations of liver tumors to 24-h post-procedure (T = 24) volumes. While ablation volume expansion was not uniform and difficult to predict, all cases demonstrated an increased volume after 24 hours.
• Opposed to using the effective treatment volume, the authors from Brown University (Providence, USA) publishing "Prospective Margin Estimates Predict Local Tumor Progression Following Microwave Ablation of Small Renal Masses" used the planned treatment volume within the computation pipeline. This refers to the ellipsoidal volume provided by the ablation device manufacturer based on the user-selected energy settings. This volume is then mapped onto the tip of the instrument as visible in control CT imaging. The resulting annotations are then put into relation with pre-operative generated kidney and tumor annotations. The analysis revealed a significant association between the risk of local tumor progression and smaller estimated margin sizes, as indicated by the first quartile (Q1; 25th percentile), maximum, and average measurements of ablative margins.
• Finally, at the forefront of margin assessment developments, the ACCLAIM trial marks a significant milestone. This prospective, multi-center, standard of care trial aims to demonstrate that MWA of liver lesions will result in a 2-year local progression free survival of at least 90%. Integral to this study is the requirement for post-ablation 3D margin assessment. This research is still in its early stages, with the primary endpoint expected to be reached in 2027, yet it already presents an exciting advancement - again proving significant legitimate physician interest in the topic.
Precise alignment of the intraprocedural CT images is imperative to assess the ablation margins. This is particularly important as any change in the patient's position can alter the anatomy of the target area. With the CAS-One IR workflow, deformation artifacts caused by patient movement and breathing is minimized with stabilization and respiration control techniques. Despite these advances, one major obstacle remains for all methods: the effective compensation of complex deformations caused by significant contraction when treating subcapsular tumors.
The fact of ablation volume increase during the post-ablative course adds an important piece of evidence for clinicians to consider during the assessment of the treatment. However, due to the existence of impacting factors such as nearby vessels causing a heat-sink effect, ablation volumes show a non-uniform increase, thus making it difficult to predict while the patient is still on the table.
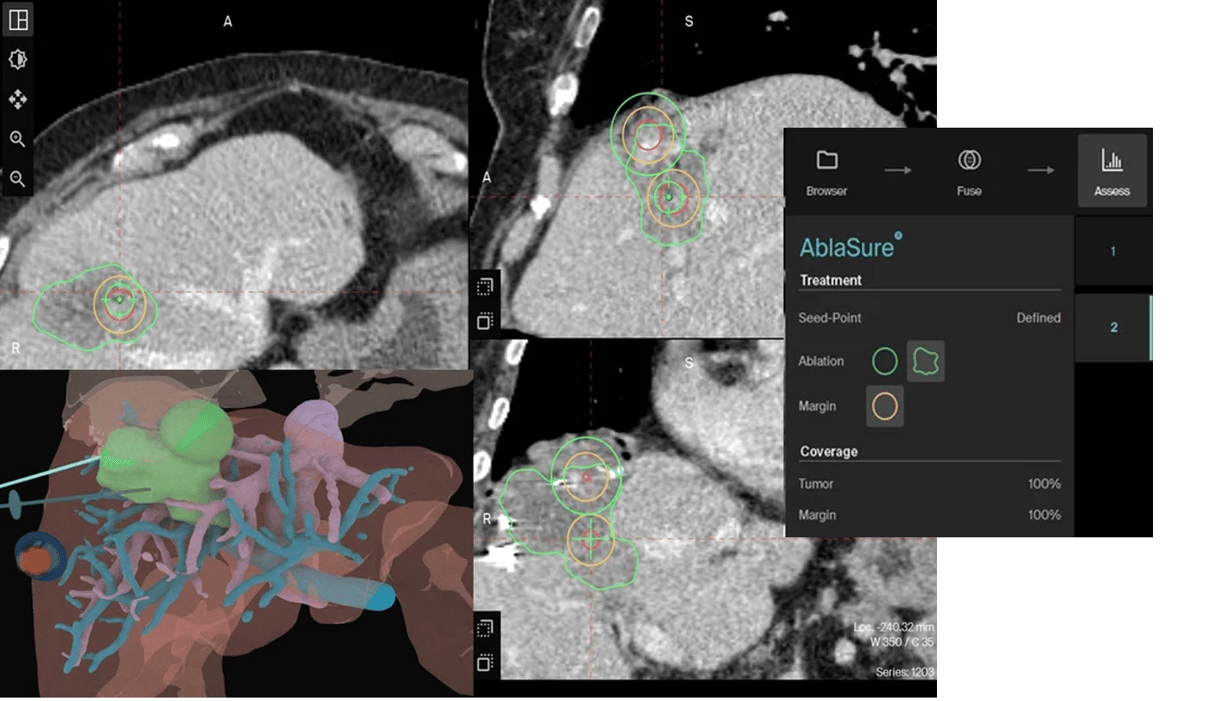
Our AI-driven AblaSure feature already enables the quantification of effectively achieved margins from images before and after the ablation. This calculation is done in less than 10 seconds while the physician remains at the patients side after the procedure - enabling them, to make an immediate decision to re-ablate if necessary. The integration of the planned treatment volume to prospectively “predict” the margins states an interesting addition. This would empower clinicians to quantitatively evaluate the discrepancy between planned and actual margins obtained post-ablation.
We will keep ourselves informed as more and more peer-reviewed publications become available on this exciting, and fast moving topic.